When the Emergency Department is the emergency
The universal (negative) ER experience, the companies attempting to address it, and how AI can shift the paradigm
Think back to the last time you were in the Emergency Department (ED). Did you feel your experience was pleasant? Sufficient? Did you feel cared for? If your answer to any of these questions was “no,” you are not alone. Interestingly, “a patient's ED experience is largely based on their perception of their doctor.”1 Given that providers are highly skilled and well-educated professionals, we must wonder what might lead patients to have a bad “perception” of them. This is obviously a multivariate problem; however, we would argue that it can be distilled down to one common denominator: time. Providers are not given enough time to truly “care” for their patients. ED providers in particular, don't have time to be empathetic, they don't have time to get to know the patient on a more personal level, and they don't have time to allow humanity to distract from care delivery.
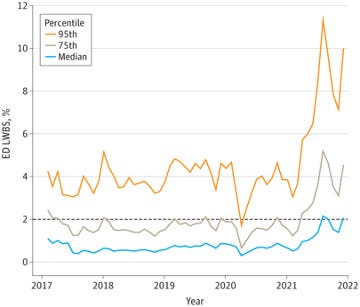
If you look around and start to peel back the onion of operations in an ED setting, you won't have to look very far to uncover the countless inefficiencies that exist in this one part of a hospital. These inefficiencies coupled with the surge of ED patient volumes over the past several years has left providers overworked and burnt out, leading to less-than-optimal patient experiences. In fact, a Yale study from 2022 found that ED overcrowding has led to rates of patients who left without being seen nearly doubling from 2017 to 2021.2 This is where technology can help. When used appropriately with human oversight, recent advances in technology have the potential to reduce the non-patient care work providers are tasked with, reduce operational inefficiencies in the care journey, spot incidental findings, assist patients in understanding their issues, and help ensure continuity of care in ways that were never feasible before.
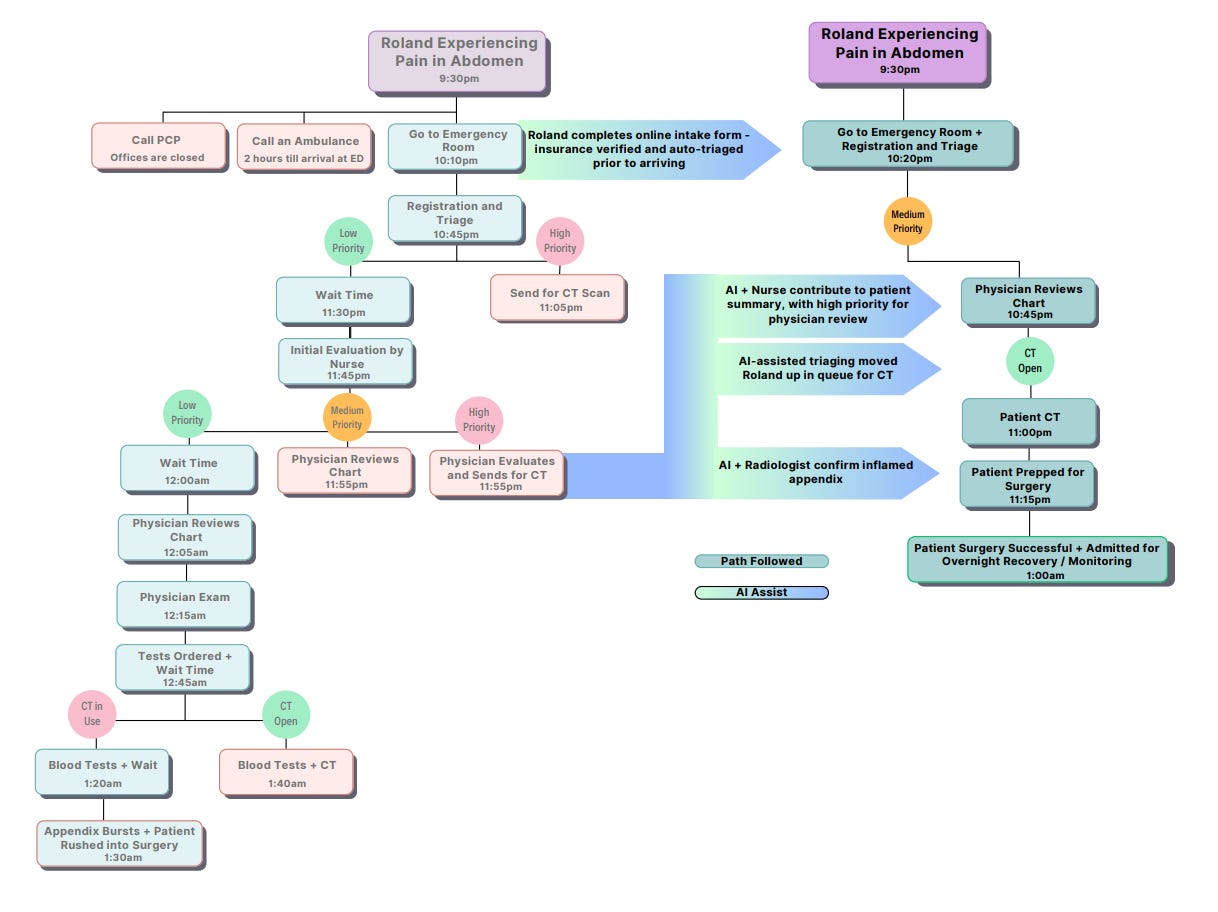
Don't just take our word for it. Let’s take you on a journey through a fictional ED visit. First, we will travel this journey as it currently exists, with minimal assistance or guidance from technology. Then, we will go on the same journey in a tech-assisted setting. Before we get to that, let’s take a step back and see where EDs, as we know them today, came from.
History of the Emergency Department
Emergency medicine is a relatively new specialty, having been approved and recognized by the American Board of Medical Specialties (ABMS) in 1979. This followed high demand for emergency medicine services and a lack of infrastructure to support patients needing immediate care at hospitals. Before emergency medicine became a specialty, hospitals had emergency rooms that were staffed with rotating clinicians and broadly uncoordinated care, often leading to poor health outcomes.
After the ED was established formally, it gained popularity in the 1990s particularly with the development of media in the form of movies and television shows (like “ER”) that revolve around emergency medicine. Emergency rooms experienced increased demand alongside urbanization, which was fueled by increased public awareness of this line of care.
There were an estimated 139.8 million emergency department visits in 2021, up from 124 million in 2009 and 90.3 million in 1996 (this is a 55% increase from 1996 to 2021!). 34 Obviously, there is continued demand for emergency room services; in many cases, patients have defaulted to EDs as their primary site of care. This has led to crowded (and often unpleasant) EDs that are filled with patients who must endure long wait times and burnt out clinical and administrative staff. Further evidencing how many eyes are now on ED performance, efficiency, and patient outcomes, the Senate just announced an investigation into private equity involvement in EDs. An estimated ~40% of EDs are run by companies owned by PE funds, and the investigation is specifically aimed at understanding how care quality and provider wellness has been impacted by PE involvement in EDs.
Augmenting Emergency Medicine with Technology
The inefficiencies facing modern day EDs can be in part addressed by technology used to alleviate administrative burden and ease the process of visiting the emergency room for a patient. Companies like Fabric Health and CyrenCare are helping with intake and triage of patients across care settings, including the ED. Other solutions target time-consuming administrative tasks. For example, ambient listening companies like Abridge have received a lot of attention from venture funds recently. Other companies like RightSite are trying to reduce the amount of avoidable ED visits by providing on-demand care coordination and potential diversion to more appropriate sites of care. There are also several hospital systems that offer virtual urgent care and emergency care directly to patients. In general, we expect the trend of technology-assisted ED processes to continue to rise over the coming years, both helping to alleviate burnout and reduce avoidable visits where possible via virtual care and the incorporation of AI-assisted chat technology.
Post-admission, data shows that ~50% of patients receive some kind of imaging in the ED.5 This creates yet another administrative and process burden for ED staff and providers. There are many companies tackling the radiology space, a service line which is no stranger to leading the pack on technology adoption. Companies are targeting radiology inefficiencies from all angles, such as optimizing the use of imaging equipment (e.g., Quantivly), automating impressions and / or generating clinical findings (e.g., aidoc, Rad AI, RapidAI), and generating reports for care teams and patients (e.g., Scanslated). These companies can help patients get faster diagnoses while reducing the amount of time providers need to spend with each patient, in turn increasing the capacity of imaging technology, allowing for more scans and increased revenues for hospitals.
Now that you have an idea of the breadth and depth of the problem space, and (hopefully) at least a general understanding of how companies are trying to position technology to tackle it, let's see firsthand how these new technology-assisted EDs compare to EDs of today. To do this, we’ll follow a fictional patient on his journey through each of these care settings.
Today’s ED Visit
Meet Roland. Roland is a 40-year-old male who has been experiencing lower right abdominal pain increasing in severity over the last 24 hours. The pain began shortly after Roland finished several servings of Moira’s Famous Folded Cheese Enchiladas. Roland ‘s wife, Jocelyn, finally convinces him that it is time to go to the emergency room to get checked out. They jump in Roland’s truck and head over to Elmdale General.
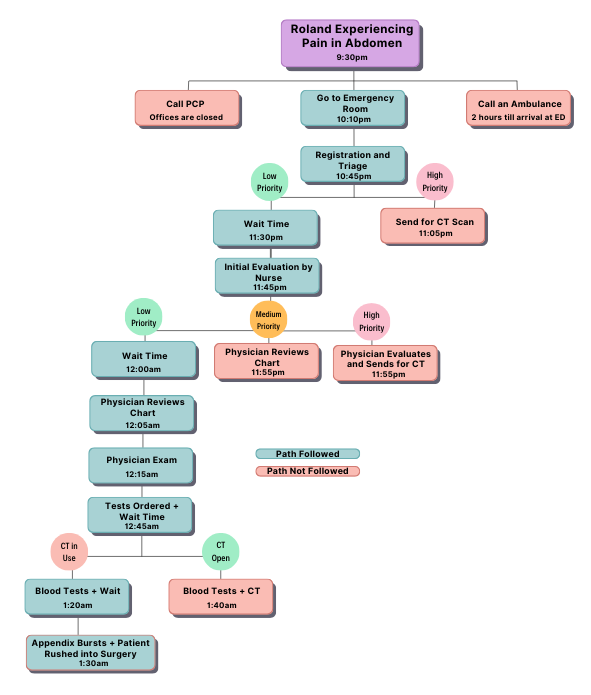
The above takes us through a potential ED visit today (keep in mind, this is hypothetical but very possible), not augmented by any AI assistance.
Upon arrival, Roland undergoes triage and has to fill out a manual registration form, providing medical history, current medications, symptoms, and of course, insurance information before anything else. Because the ED is so thoroughly crowded, there are no available rooms, and Roland is placed onto a bed in the hallway, while Jocelyn anxiously waits with him. A nurse who is currently caring for 7 patients at once performs a brief assessment of Roland. Because Roland appears to be stable, he is classified as low priority and must wait for the next available physician.
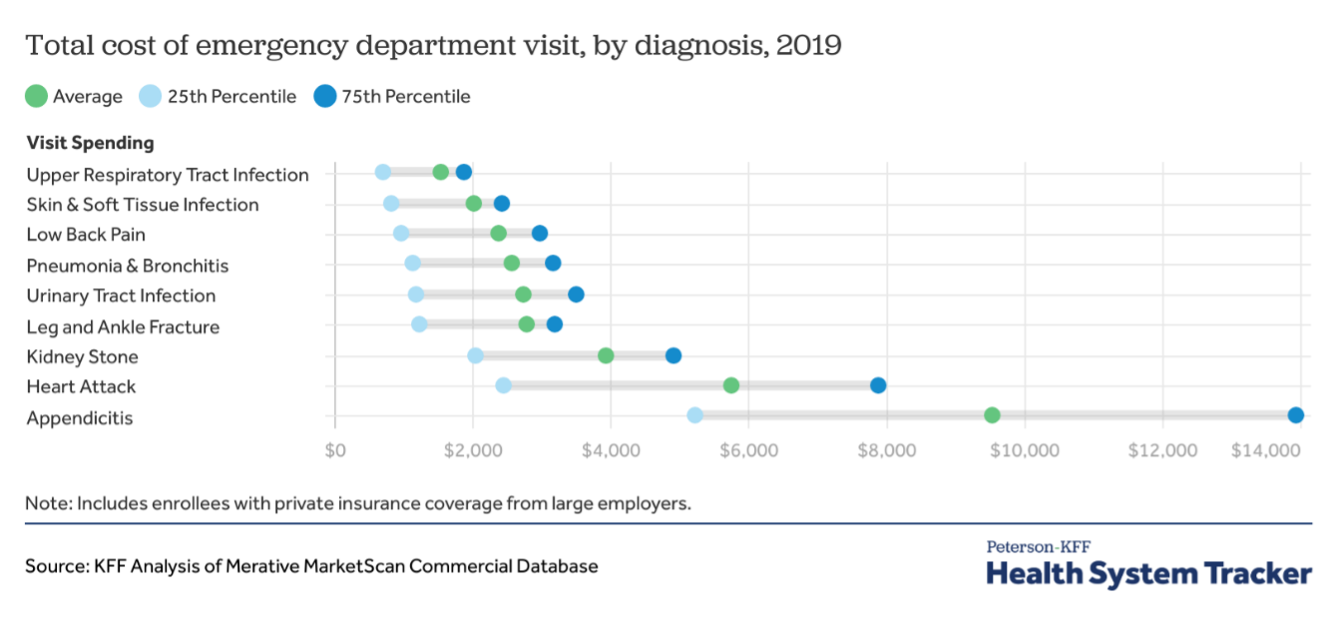
Roland and Jocelyn wait for over an hour as the physicians are overwhelmed with patients. The physician quickly introduces themselves to Roland and performs an exam, noting pain in the right abdomen. The physician decides to send Roland for a CT scan and to perform bloodwork. Because it is unclear which is to occur first and the CT scanners are all in use, Roland is told he must wait for a nurse to draw his blood. Roland and Jocelyn wait for another hour. As Roland is being wheeled up to Imaging, his pain becomes severe and his appendix bursts. He then has to be rushed into a more invasive open appendectomy.
So much of what goes into that frantic rush to the ER is decision-making at the patient, caregiver, and / or bystander level. Deciding to seek out care is just the first step. With the recent uptick in urgent care centers, the hesitance to face an exorbitant ER bill, the assessment of if a call to 911 is necessary, and the layperson’s triage that puts all these realities into motion, deciding on the “right” path to care is enough to turn any emergency situation into a full-blown disaster.
At the end of the day (because let’s be honest, that’s typically and frustratingly when you need to go to the ER instead of daylight hours when your PCP’s office is open), you have to be the one to make the call. Take our friend, Roland. He and Jocelyn decide to go to Elmdale General, but that’s at least 30-40 minutes away from where they live. There’s no time to wait for an ambulance and maybe they could visit the local vet in lieu of urgent care, but the reality is that it’s a combination of luck and timing whether or not Roland’s appendix bursts before they make the drive. Once they arrive at the ED, due to only the circumstances of overcrowding, burnout, and inefficient resources, Roland and Jocelyn enter a loop of being seen and being made to wait for hours. By the time his condition drastically worsens, it’s already too late. It all comes down to decision-making. And if there’s one thing we consistently turn to AI for in healthcare, it’s decision support.
A Future ED Visit
Meet Roland. Roland is a 40-year-old male who has been experiencing lower right abdominal pain increasing in severity over the last 24 hours. The pain began shortly after Roland finished several servings of Moira’s Famous Folded Cheese Enchiladas. Roland ‘s wife, Jocelyn, finally convinces him that it is time to go to the emergency room to get checked out. They jump in Roland’s truck and head over to Elmdale General.
The above takes us through a successful ED visit augmented by AI. Everything you see here is attainable by year’s end if health systems are willing to implement these solutions efficiently.
Prior to even arriving at the ER, Roland is able to use the AI-assisted intake tool built into his provider app to complete registration, insurance verification, and intake forms while en route to the hospital. Triage staff in the ED will be able to meet him upon arrival with his patient wristband prepared. The intake / triage nurse will verify the prioritization that AI has recommended based on Roland’s symptoms recorded in the intake form. The nurse will be able to have a real, human conversation with Roland, maintaining eye contact and conveying a sense of empathy for the person in front of them, while AI transcribes the intake note for them (completely ambiently). The intake nurse will then read through the note, correcting / augmenting where necessary and queue Roland up for a visit by a physician or APP. This queue will be maintained largely by AI, prioritizing patients based on predicted necessity learned by analyzing similar cohorts of patients. This prioritization can be conveyed via a continuously updating dashboard at the Nurse Manager’s station. A single human can confirm these recommendations and more intelligently and efficiently schedule resources.
The physician will then have a similar experience. They will pick a patient from the list in the order provided to them, be brought up to speed on the case with a concise descriptive summary of the patient intake (generated by AI). The physician will then use speech-to-text to leverage their personalized AI assistants to help answer any other questions they may have about the case before stepping into the exam room with Roland. This interaction would also be very human, relying on transcriptive AI, operating ambiently in the exam room, to compile the transcript for approval by the physician and input into the chart. The physician will note on the patient chart that both the AI and nurse have flagged fever, nausea, and right abdomen pain as cause for concern, potentially indicating gastroenteritis or appendicitis.
Roland will be sent for a CT scan immediately to confirm, where his case will be prioritized by AI in the Radiology system(s), performed by a technologist with positioning and contrast recommendations generated by another AI-enabled tool. Jocelyn is able to get real-time updates of Roland’s status through the patient portal, which notifies her once his imaging has begun. This imaging will then be sent through a suite of AI tools ensuring that there are no incidental or urgent findings necessitating immediate intervention. The case is then prioritized accordingly on the Radiologist’s reading list, where physicians will interpret the scan (likely pre-produced in part by AI) and transcribe a report ready for review by the patient’s primary ED physician. Again, this report will be sent through an AI screening mechanism to check for errors in the report (laterality, etc.) and ensure there is nothing urgent, caught by the Radiologist, that needs to be brought to the ED physician's attention immediately. Assuming nothing urgent is flagged and the physician can diagnose as food poisoning, AI will generate a discharge summary and the physician will go over Roland’s treatment plan, including fluids and cautionary medication. Alternatively, and more crucially, if the scans reveal an unusually inflamed appendix, this gets alerted up the proper channels automatically, and the patient can be prepped for a less invasive laparoscopic surgery in a timely manner.
We want you to take specific notice to how AI assists with this visit. It removes the non-human tasks, helps to lower the impact of human error, and expedites decisions faster than humans ever could. Whereas without AI, Roland was rushed into surgery with a burst appendix at 1:30am, with AI assistance embedded throughout the ED workflow, Roland is already in the post-surgery recovery room by 1:00am. Never in this scenario is AI given the ability to treat a patient or make a medical recommendation without including a practitioner. This is where the beauty in the symbiosis between human and machine exists. This is what we must optimize for.
Which Would You Prefer?
We don't think it's a bold assumption to expect nearly everyone to prefer the experience offered in a future-state world. Luckily for those in this camp, this world is not too far away. We spoke to three individuals about this to get their candid feedback. Here’s what they said. (Okay fine, full disclosure, theses statements were produced by Gemini. However, they are directionally reflective of candid, qualitative feedback we have encountered over the last year or so.)
Patrick:
"I'm excited about the potential of AI to improve my healthcare experience. It could help providers make more accurate diagnoses, personalize treatments, and monitor my health more effectively."
Johnny Rose:
"While I appreciate the benefits of AI, I'm cautious about its potential impact on the patient-provider relationship. I want to ensure that AI is used as a tool to enhance care, not replace the human connection."
Stevie Budd:
"I'm optimistic about AI's ability to make healthcare more accessible and affordable. However, I urge providers to prioritize data privacy and transparency. I want to know how my data is being used and have control over its use."
One of the unique elements of healthcare as an industry is that every single person, whether they work in healthcare or not, is a subject matter expert at being a patient. Likely, each and every one of us has had some sort of ER experience similar to Roland, and it doesn’t take a degree or a long career in this field to know change is desperately needed. What better place to implement that change than at a key entry point for so many patients: the Emergency Room. As is hopefully evident by the above feedback patients gave when asked about allowing AI to assist in their care delivery, people seem to be ready for this. AI has already made a positive impact (when used appropriately) in people’s everyday lives. So long as they are implemented appropriately and used ethically, enabling providers to leverage these powerful tools seems to be viewed as a win-win by society.
Final Thoughts
Although this story was simplistic in nature, it is very real. The care systems as they are currently implemented are ripe for innovation. Most hospital systems worth their salt are beginning the shift towards this artificial intelligence assisted workflow paradigm as we speak. The adoption curve is slower than in most other industries, given healthcare’s unique challenges surrounding regulatory and compliance concerns, resistance to change, data quality and interoperability challenges, and resource constraints, to name a few. However, we strongly believe that EDs (and patient care systems, more broadly) that do not implement this new technology-assisted paradigm will have worse patient outcomes and higher costs of care than ones that do. This may very well turn into a war of attrition, but eventually, EDs as we know them today, will be a thing of the past.