desert-ED
Sand, sand, and more sand - the dunes of healthcare
What is a healthcare desert?
Healthcare deserts (also known as medical deserts), not to be confused with actual deserts, are defined by the WHO as “geographical areas where populations have limited access to qualified healthcare providers and quality healthcare services.” This can include essential healthcare such as primary care, specialists, community health centers, and emergency medicine. Healthcare deserts are typically characterized by a scarcity of healthcare facilities and providers, which is often due to low population density, economic challenges, and workforce shortages. While rural locations are often healthcare deserts, urban areas with high poverty rates can also experience similar lack of connectivity and availability of healthcare resources. Medical deserts are often impacted by socioeconomic factors such as affordability of care, health literacy, and access to the internet, leading to the continuation of health disparities.
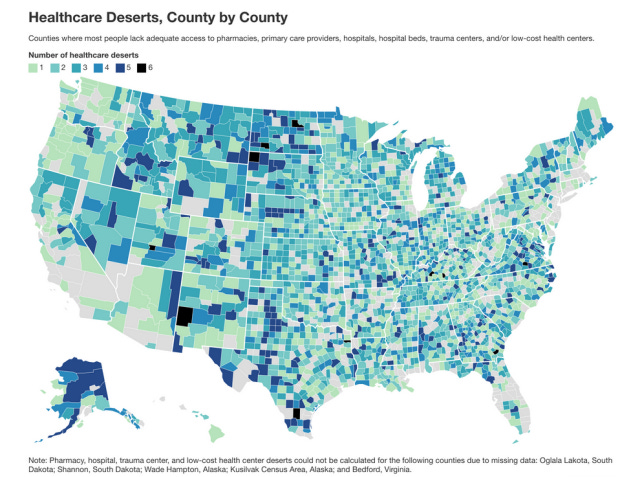
An estimated ~80% of American counties do not have adequate healthcare infrastructure. Residents of medical deserts often face long travel distances to reach the nearest healthcare provider and / or pharmacy, which can lead to avoidance or delays in receiving care and poorer health outcomes. These patients are not able to have regular checkups with a PCP and are therefore more likely to die from preventable and / or chronic conditions. An analysis done by the National Center for Health Statistics showed that mortality rates for residents of rural populations between the ages of 25 and 64 rose by 12% from 1999 to 2019; during the same period, overall mortality rates for Americans decreased. Additional troubling statistics about healthcare deserts and rural communities in the US include:
Residents in 40% of counties must drive more than 15 minutes to the closest pharmacy
20%+ of counties are hospital deserts where people need to drive more than 30 minutes to the closest hospital
47% of counties have fewer than 2 hospital beds per 1,000 people
40%+ of counties are trauma center deserts where people need to drive more than an hour to a hospital that can handle traumatic injuries
45%+ of counties are low-cost health center deserts where people need to drive more than 20 minutes to an FQHC
~66% of Primary Care Health Professional Shortage Areas (HPSAs) are located in rural areas
GoodRx did an analysis of healthcare deserts and identified geographies across the US that have inadequate access to healthcare resources, as shown in the map below. They estimated that ~121 million Americans currently live in a county classified as a healthcare desert.
Technology challenges
Although technology-enabled care such as telehealth and mobile health solutions offer promising ways to address healthcare access issues in healthcare deserts, there are a tremendous amount of technology-centric issues stemming from these regions. Technology basics such as internet connectivity, digital literacy, access to devices (such as smartphones, tablets, or even laptops) are often lacking. More nuanced issues such as provider adoption of technology, data security and privacy issues due to a lack of qualified technologists to implement robust systems, and other cultural barriers add yet another layer to this issue. For deserts that fought upstream and broke through these barriers, a new issue arises: integration. Integration is extremely difficult even for the most connected hospitals and health systems. When you layer on the lack of adequate talent resources, limited desire to implement, and funding issues, integration becomes a nearly impossible task. This leaves the technology these systems can implement in a siloed state, severely limiting their effectiveness.
The Big Apple (a day really does keep the doctor far away)
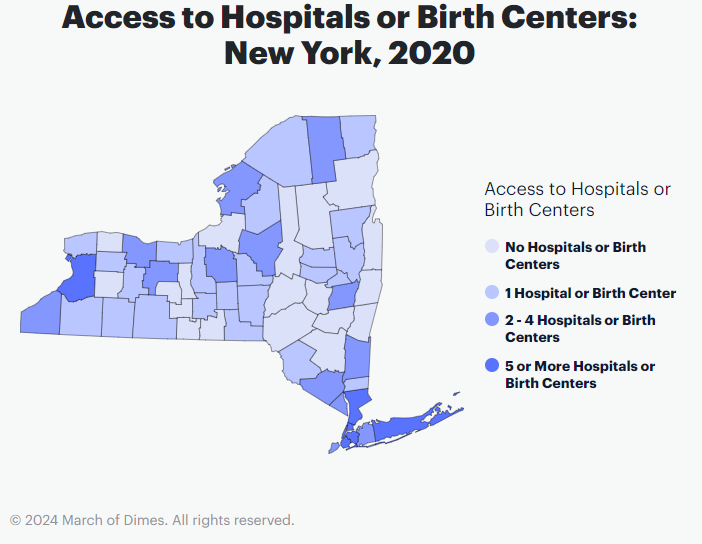
There tends to be a mindset that healthcare deserts are isolated to isolated regions, certainly not by the coasts, and certainly in some faraway barren landscape. The reality is that many identified healthcare deserts might be closer than you think. In fact, approximately 36 out of 62 New York counties are considered primary care deserts, affecting 3.1 million residents. When considering maternity care deserts, 3.2% of New York counties are considered maternity care deserts and 8.1% of counties have low or moderate access to care, per a recent March of Dimes analysis.
In many New York counties, people lack access to crucial medical services, such as pharmacies and local trauma care. Our longtime readers might recall when Roland from our Emergency Departments article had to travel all the way to Elmdale General Hospital late in the evening. These are the kinds of access issues that can mean life or death. One New York county identified as a healthcare desert, Cattaraugus County, has only 2 hospitals, the larger of the two with only 186 beds. This past year, Kathy Hochul, Governor of New York, announced initiatives to improve healthcare across the state. New York currently ranks 28th in the nation for providing prevention and treatment-based health care. These gaps in care access also very disproportionately affect those in marginalized communities as well as Medicaid program participants. As such, Governor Hochul intends to increase Medicaid rates for providers taking part in the Patient-Centered Medical Home model. The initiatives also include support for mental health services integrated with primary care and adjustment of reimbursement rates. In a similar effort, a bill was recently introduced by Senator Michelle Hinchey and Assemblywoman Nily Rozic, called the Hospital Transparency Act. A key goal of the bill is identifying healthcare deserts by requiring hospitals to inform patients of the types of care services they provide. This ensures transparency regarding certain services where there are clear gaps, such as abortion access and gender-affirming care. The bill has passed in both the State Senate and Assembly.
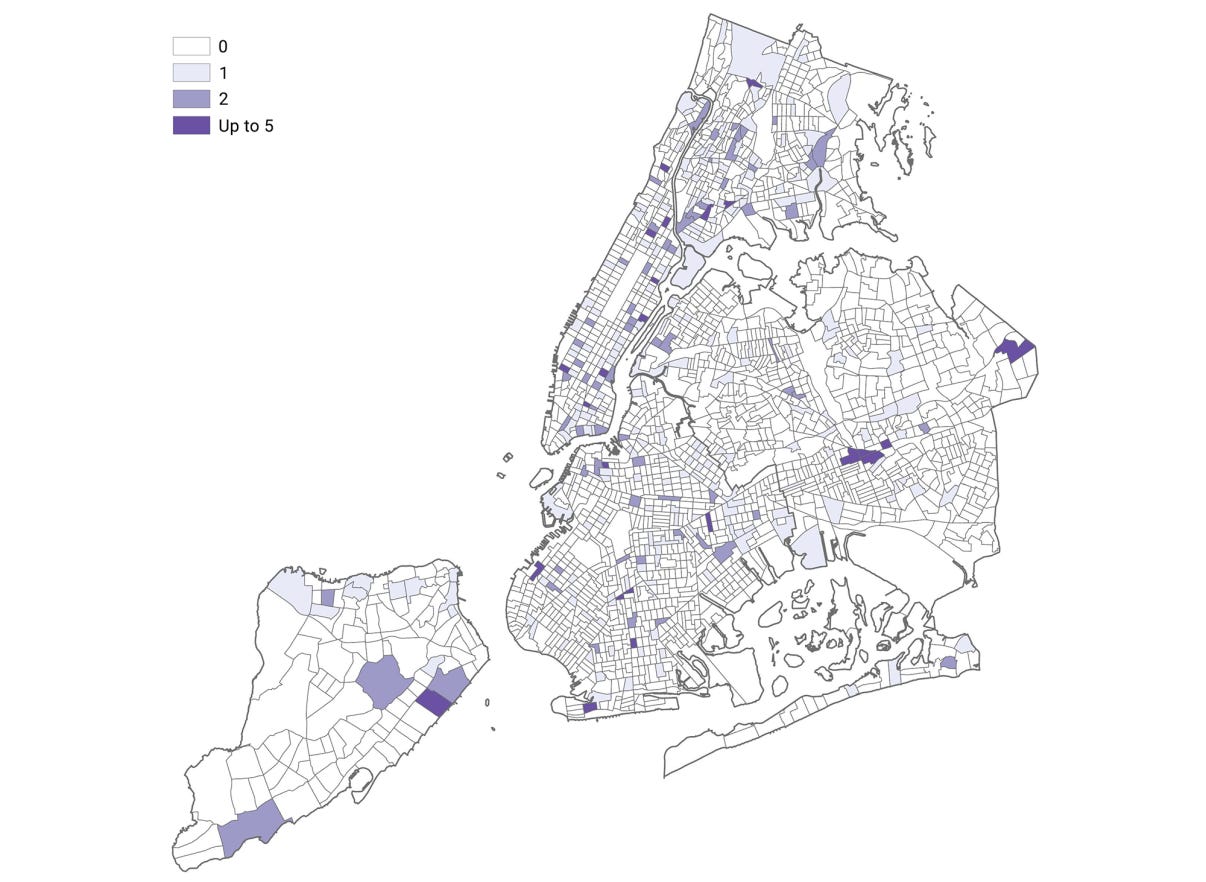
It’s one thing to think of New York as a state having pockets of healthcare deserts, but surely not NYC, our concrete jungle where dreams are made of? Turns out there may be some more sand in the cracks of that concrete than expected. Due to healthcare worker counts being significantly higher in certain boroughs like Manhattan and the more scattered placement of healthcare facilities in various neighborhoods, many of these areas without access have effectively become healthcare deserts. Of the healthcare facilities providing some sort of primary care service, the majority are found in Manhattan and Brooklyn, with Queens and the Bronx often being underserved. Many areas are also lacking affordable and timely transit options, creating another barrier to care access. Between the fallout from COVID-19 with respect to jobs and burnout as well as the existing racial, ethnic, and socioeconomic disparities that impact care access and delivery, it is more important than ever before to assess and mitigate the existing care gaps across New York and beyond.
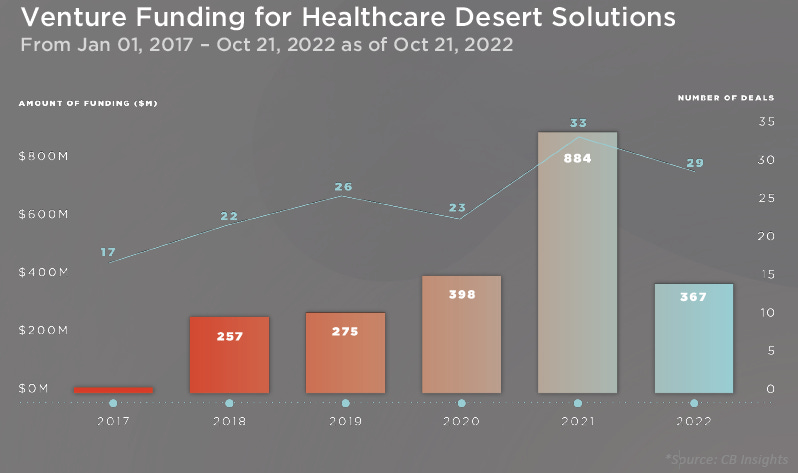
Companies addressing care access in these areas
There are venture-backed companies that are beginning to build innovative solutions to address the clear gaps in care that exist because of healthcare deserts.
Companies like Hamilton Health Box are building microclinics that combine in-person care with technology to extend geographic reach. They are partnering with providers, payers, and employers to lower the overall cost of care by increasing member engagement and expanding provider networks via small footprint models. Homeward Health is also focused on extending care accessibility for rural Americans through clinics in Minnesota and Michigan that combine in person services with virtual and home care for Medicare patients. Similarly, Main Street Health is focusing on value-based care offerings in rural America. Backed by Oak HC/FT as well as several large national Medicare Advantage plans and provider partners, Main Street Health is scaling quickly across the US. Cityblock has been at the center of providing value-based care to Medicaid and lower-income Medicare beneficiaries for several years. The company has a special focus on geographic areas catering to these populations, which are oftentimes healthcare deserts and / or rural communities.
Healthcare deserts are plagued with myriad care access limitations, one of the key issues being transportation. Many healthcare deserts are in rural areas and are already subject to long travel times for inpatient care specifically (average of ~24 miles to a hospital vs. ~3 miles in non-rural settings). To account for sparse emergency transportation and hospitals, many efforts are being made to incorporate non-emergency medical transportation (NEMT) options. Companies like Uber and Lyft have incorporated healthcare options that give patients access to rides and deliveries of prescriptions or groceries, for instance. Uber works with care coordinators through their HIPAA-compliant solution to ensure patients get to their appointments and get the assistance they need. Lyft even highlights offering rides to fitness appointments and partnering with payers to provide NEMT to commercial, Medicare Advantage, and Medicaid members. Lyft also partnered with SafeRide to create a more seamless, end-to-end patient experience for their medical transportation.

While these companies are specifically targeting care deserts and rural communities, there are countless virtual care and remote monitoring businesses that have come about and gained popularity, in part fueled by the need to extend telehealth capabilities during COVID-19. While these companies are attempting to reach patients in medical deserts, many of the residents in medical deserts do not have access to the internet and therefore cannot benefit from virtual care. In Mississippi, New Mexico, and Arkansas, nearly 20% of households do not have internet access. This directly impacts the effectiveness of telemedicine given a large subset of these populations cannot access care in a virtual way.
The high cost of living in a healthcare desert
Imagine struggling to breathe because of a persistent cough, or facing the daily struggle of managing diabetes, but finding it nearly impossible to get the medical care you need. This is the heartbreaking reality for millions living in healthcare deserts – areas starved of essential medical services. The consequences are devastating.
Residents of healthcare deserts are more likely to succumb to preventable and treatable conditions like heart disease, stroke, and diabetes. This is largely due to delays in receiving care, lack of preventive services, and the inability to effectively manage chronic illnesses. Chronic diseases become a ticking time bomb in these underserved areas. Without regular monitoring and management, conditions like hypertension and asthma spiral out of control, leading to complications, hospitalizations, and tragically, premature deaths. This lack of access ultimately contributes to a lower life expectancy for those residing in healthcare deserts. The absence of readily available preventive care further exacerbates the problem. Routine screenings, vaccinations, and wellness check-ups are vital in detecting and addressing health concerns before they escalate. However, these services are often scarce in healthcare deserts, leading to higher rates of preventable diseases and late-stage diagnoses, where treatment options are limited and significantly more expensive.
The impact on maternal and infant health is particularly concerning. Limited access to prenatal and postnatal care translates to a higher risk of complications during pregnancy and childbirth. Conditions like pre-eclampsia and gestational diabetes may go undetected and untreated, jeopardizing the well-being of both mother and child. By 2030, the supply of OBGYNs in rural areas is expected to meet only ~50% of the demand in those regions, which can lead to even poorer maternal and infant health outcomes.
The lack of access extends beyond physical health, casting a shadow on mental well-being as well. Healthcare deserts often lack adequate mental health services, leaving individuals struggling with depression, anxiety, and substance abuse without proper support. This can have severe consequences, increasing the risk of suicide and other mental health crises.
Living in a healthcare desert takes a significant toll on quality of life. The constant worry of untreated conditions, the stress of navigating a fractured healthcare system, and the feeling of being left behind all contribute to diminished well-being and reduced productivity.
Continuity of care (lack thereof)
Even when you see a physician, the challenges faced in healthcare deserts almost always result in this visit being siloed, having no continuity of care to follow. Provider shortages often force patients to see different doctors, hindering the development of trusting relationships crucial for effective care. Limited access to specialists and inadequate transportation options further disrupt care plans, leading to delays in follow-up appointments and specialized treatments. Fragmented medical records due to a lack of integrated EHR systems create gaps in care, while economic constraints prevent many from affording regular visits, pushing them towards costly emergency care. While telehealth offers promise, limitations in its scope and technological barriers like poor internet access hinder its effectiveness. These challenges are compounded by lower health literacy rates, making it difficult for patients to fully grasp treatment plans and adhere to them. The lack of essential healthcare infrastructure, including pharmacies and rehabilitation centers, further impedes timely diagnostics and comprehensive care management.
Conclusion
Healthcare deserts have become a staggering and pervasive problem across the United States, affecting a significant portion of the population. The causes stem from low provider / facility availability, archaic or absent technical infrastructure, and lack of transportation options, among other systemic issues. While certainly prevalent in rural areas, medical deserts exist all across the country, affecting cities like Los Angeles and New York. While legislation is being considered and passed to address these gaps in care, many companies are making it their mission to address the rise in healthcare deserts through innovative and creative solutions to bring affordable care to those in need. There is certainly a long way to go and though comprehensive access to care regardless of location and sociodemographic status feels more like a mirage than a reality, hopefully we continue making strides in the right direction.